Doctors want you to stop doing two things: eat junk and google your symptoms. We know it’s easier said than done. You are going to think about a snack when it’s 4 pm and you are tempted to look up something very mild online and find out that you have AIDS.
To solve the second issue, we looked for the 10 most common questions people have about a growing health risk or disease and let our doctors give you verified answers. We’ve all suffered from the IDIOT syndrome. Let’s put an end to this.
To start this series, Even doctor, Dr Rakshith Shetty answers 10 Most Googled Questions About Type 2 Diabetes
What is the difference between Type 1 and Type 2 diabetes?
Type 1 Diabetes (T1D)
Type 1 diabetes is a chronic autoimmune disease where your body’s immune system starts to attack and destroy insulin-producing beta cells in your pancreas.
The aetiology of T1D is multifactorial and involves a complex interplay between genetic and environmental factors. One key genetic risk factor for T1D is the presence of specific human leukocyte antigen (HLA) alleles, such as HLA-DR3 and HLA-DR4, which are associated with an increased risk of developing T1D.
Some research shows that the immune system is triggered by most notably enteroviruses (EV) and is trying to destroy a virus but due to molecular mimicry (where viral proteins resemble the beta cells’ proteins), it ends up attacking the beta cells as well. However, not everyone with Type 1 diabetes has a clear viral trigger, and the exact causes of the autoimmune response can vary. Genetics and environmental factors also play significant roles in the development of the condition. Since viruses can often trigger autoimmune diseases, experts are studying whether the Covid-19 pandemic had significant impact on the development of autoimmune diseases. The long-term effects of COVID-19 infection on T1D are under study presently.
People with Type 1 diabetes often need to take insulin injections or use an insulin pump.
Type 1 diabetes usually develops in children or young adults, but people of any age can get it.
Type 2 diabetes
This is a metabolic disease and the most common type of diabetes, which occurs when the pancreas do not produce enough insulin or the body’s cells don’t respond properly to insulin.
This can be caused by a number of factors, including lifestyle factors like obesity and lack of exercise, as well as genetic factors.
People with Type 2 diabetes may take medications to help their pancreas produce more insulin, their liver release less glucose, or their cells use insulin more effectively or manage it through diet and an active lifestyle modification.
What are symptoms and risks associated with Type 2 diabetes?


Can Type 2 diabetes be reversed?
It is important to make a clear distinction between diabetes reversal and diabetes remission. Diabetes cannot be cured/reversed and there is no guarantee that it can go away permanently. But with regular follow ups with doctors and following an active lifestyle and dietary advice from clinical dieticians and with a well balanced diabetic diet, it can be controlled and diabetics can lead a normal life free from complications of diabetes .
However diabetes can be controlled and is said to be in remission when blood sugar levels are below the diabetes range for at least three months and you don’t need to take diabetes medication anymore. In such a case, the HbA1C levels stay below 6.5.
Even specialises in diabetes management. Our team of expert doctors and clinical dieticians have decades worth of experience in detecting early signs of diabetes, managing late stage diabetes under its Managed Care programs.
Can Type 2 diabetes be controlled without medication?
Prediabetes and early stages of diabetes can be controlled without medication under the supervision of a doctor. Healthy diet, exercise, restful sleep, maintaining a healthy weight and managing stress levels can all decrease the risk of this chronic condition.
Please note if you have diabetes, do not stop or reduce your medication if your test results show controlled levels of blood sugar. Only your doctor can advise altering/reducing/stopping your medication.
Is Type 2 diabetes hereditary?
If you have a close relative such as a parent or sibling who has type 2 diabetes, your risk of developing this condition increases. But lifestyle factors such as your physical activity, diet and body weight all influence its likelihood. Even if you have a genetic predisposition, you can reduce your risk of type 2 diabetes by managing your lifestyle.
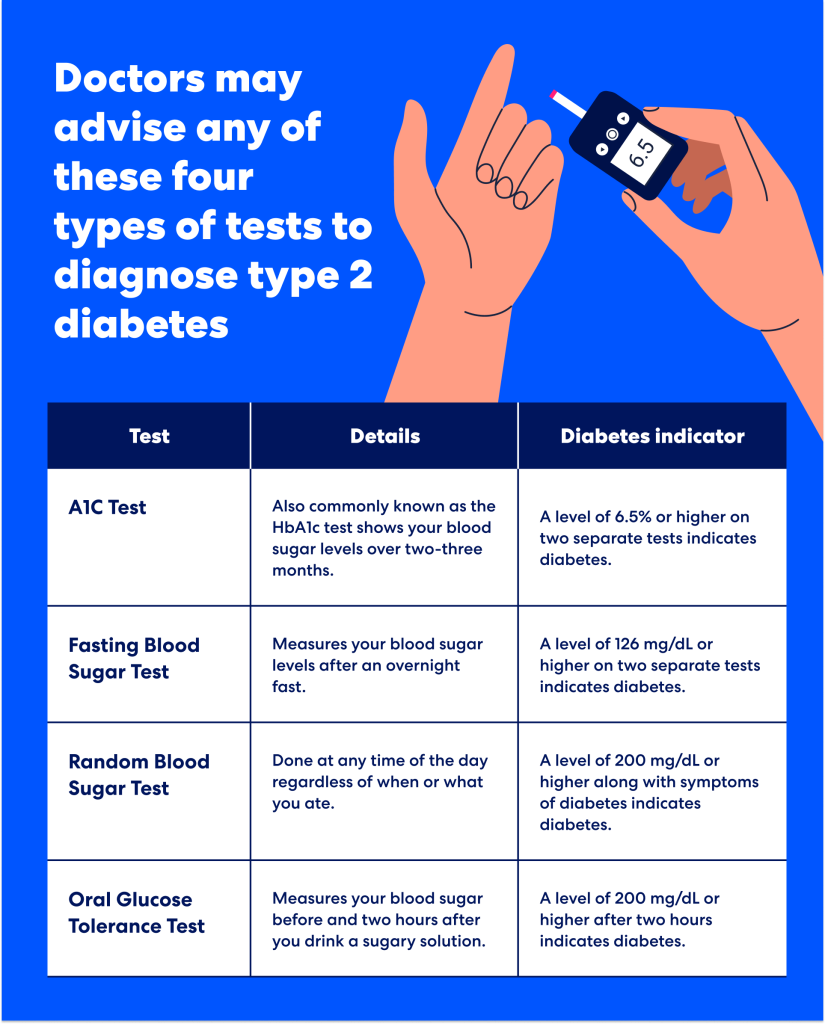
How is Type 2 diabetes diagnosed?
What is the normal blood sugar level for someone with Type 2 diabetes?
The American Diabetes Association’s goals for blood sugar control in people with diabetes are 70 to 130 mg/dL before meals, and less than 180 mg/dL after meals.
What should you eat if you have Type 2 diabetes?
A healthy diet for diabetics follows pretty much the same principles as a general well-rounded diet with some exceptions. You should opt for
Low carb food
Pick foods that are low in carbohydrates but high in healthy fats and proteins. These include leafy greens, non-starchy vegetables, nuts, seeds, avocados, and lean meats.
Nutrient-dense foods
Foods that are abundant in essential vitamins and minerals fatty fish (rich in omega-3 fatty acids), eggs, non-starchy vegetables, and healthy fats (like olive oil and nuts).
Bonus tips:
Try intermittent fasting
This should be done only under medical supervision
Personalise your nutrition
Every body reacts to the same food differently. If you can, use a CGM to understand which foods which are otherwise healthy causing a glucose spike. A clinical dietician can recommend the right diet based on your unique metabolic profile, insulin sensitivity, and other health markers.
Cook more, eat out less
Eat home-cooked meals to ensure you consume high quality ingredients and can control portion sizes. Restaurants often use high quantities of fats, sodium and often portion sizes are either inadequate or more than what you need. Choose baking and grilling over deep frying food.
Eat at the same time
It’s not just what you eat, but when you eat it. Eating carbohydrates earlier in the day rather than at night can improve blood sugar control. The body’s insulin sensitivity tends to be higher in the morning and decreases throughout the day, so consuming more of your carbs earlier can help manage blood glucose levels more effectively.
Try resistant starch
Resistant starch is a type of carbohydrate that resists digestion in the small intestine and ferments in the large intestine. This fermentation process produces beneficial short-chain fatty acids that can improve insulin sensitivity and lower blood sugar levels.
Sources: Resistant starch is found in foods like cooked and cooled potatoes, green bananas, legumes, and certain whole grains like barley.
What should you not eat if you have Type 2 diabetes?
Anything that can cause an instant spike in your blood sugar levels is not good for you.
When you consume these foods, your pancreas releases insulin to help move sugar from your blood into your cells. Over time, consuming high-GI foods can lead to insulin resistance, where the body’s cells no longer respond effectively to insulin, increasing the risk of developing Type 2 diabetes.
High Glycemic Index foods:
Refined carbohydrates like white bread, white rice, sugary cereals, and baked goods made from refined flour.
Added sugar:
Sugary drinks (sodas, energy drinks), candy, desserts, and many processed foods.
Note: You must also be careful about “no added sugar” energy bars promoted as a healthier alternative, because those offer a false sense of security and can lead to overconsumption. For example, dates are commonly used in energy bars, but dates have a high GI.
High-caloric processed foods
Not all calories are made the same. Some are indeed better than others. A mini pack of potato chips and a medium sized baked potato without toppings have the same amount of calories (around 150). However, potato chips have high sodium content and are cooked in highly saturated oil making it a poorer dietary choice.
Saturated and trans fats
Diets high in saturated and trans fats can contribute to obesity, a significant risk factor for diabetes. Examples: Fried foods, processed meats, pastries, and margarine.
Low fibre foods
Fibre slows the absorption of sugar into the bloodstream. Conversely, low fibre foods cause a rapid glucose spike in your bloodstream. Example: breakfast cereals, white bread etc.
How is diabetes and obesity connected?
Obesity is one of the most critical risk factors for developing Type 2 diabetes.
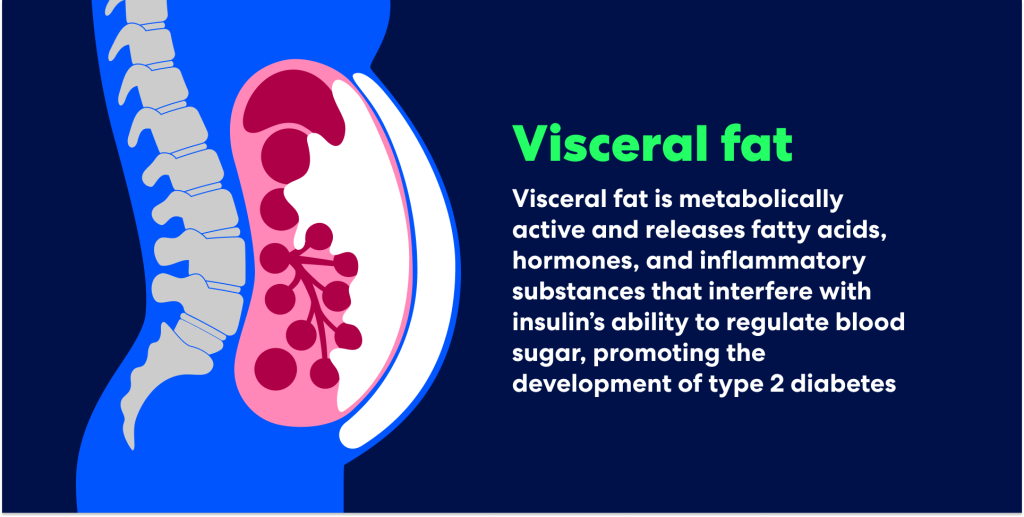
Obesity, particularly excess fat around the abdomen also known as visceral fat, can lead to insulin resistance, where the body’s cells become less responsive to insulin.
Obesity is also associated with chronic low-grade inflammation in the body. This inflammation can cause insulin resistance. The more fat tissue present, particularly visceral fat, the higher the levels of inflammation, increasing the risk of diabetes.
Note: Presence of any three of the following five conditions is essential, i.e.,for you to be diagnosed with metabolic syndrome .
- Increased waist circumference (males: ≥90 cm and for females: ≥80 cm),
- Hypertriglyceridemia ≥150 mg/dl (1.7 mmol/l),
- Low HDL (Males <40 mg/dl (1 mmol/l) and for females <50 mg/dl (1.3 mmol/l),
- Elevated blood pressure (systolic blood pressure ≥130 mmHg and/or diastolic blood pressure ≥85 mmHg or drug treatment for hypertension),and
- Elevated blood sugar (fasting blood sugar ≥100 mg/ dl (5.6 mmol/l) or drug treatment for diabetes mellitus)
How does alcohol affect Type 2 diabetes?
Alcohol is high in calories and can lead to weight gain, it can cause rapid fluctuations in blood sugar, and heavy drinking can damage pancreas and liver which are responsible for regulating insulin production and glucose metabolism
The risks and harms associated with drinking alcohol have been systematically evaluated over the years and are well documented. The World Health Organization has now published a statement in The Lancet Public Health: when it comes to alcohol consumption, there is no safe amount that does not affect health.
Got more questions about Diabetes?
Ask Even Steven! Our AI health assistant can offer medically verified answers to any health question you have. It’s FREE to use on WhatsApp
At Even, it is our job to keep you healthy and out of hospitals. Even doctors detect your health risks before they become serious illnesses needing hospitalisation.


